The ability of nurses and healthcare systems to effectively anticipate, respond to, and recover from emergencies and disasters, both natural and human-made, is a critical aspect of community health resilience. This involves a comprehensive understanding of disaster management principles, specialized training in triage, emergency care, and psychological support, as well as the capacity to adapt existing resources and protocols to meet evolving needs in crisis situations. For example, a hospital might develop detailed plans for patient evacuation in the event of a hurricane, or implement training programs for staff on managing mass casualty incidents.
Effective management of crises safeguards community well-being and reduces morbidity and mortality during unforeseen events. Historically, nurses have played pivotal roles in responding to epidemics, natural disasters, and other emergencies, highlighting the need for structured training and resources. Preparedness enhances the surge capacity of healthcare systems, ensures appropriate allocation of resources, and fosters interprofessional collaboration, thereby minimizing the impact of disasters on public health.
The following sections will explore key components of effective crisis management in healthcare, covering topics such as planning and preparation, response strategies, recovery efforts, and the crucial role of ongoing education and training.
Tips for Effective Crisis Management in Healthcare
Proactive measures are essential for mitigating the impact of disasters on healthcare systems and the communities they serve. These practical steps contribute to a more robust and responsive approach to crisis management.
Tip 1: Develop Comprehensive Disaster Plans: Detailed plans should outline specific roles, responsibilities, and procedures for various disaster scenarios. These plans must address communication protocols, resource allocation, patient evacuation, and surge capacity management.
Tip 2: Invest in Regular Training and Drills: Ongoing training ensures staff proficiency in emergency procedures, including triage, first aid, and psychological support. Regular drills simulate real-world scenarios, allowing staff to practice their roles and identify areas for improvement.
Tip 3: Establish Robust Communication Systems: Reliable communication channels are vital for coordinating responses, disseminating information, and maintaining situational awareness during a crisis. Redundancy in communication systems should be incorporated to ensure continuity.
Tip 4: Foster Interprofessional Collaboration: Effective crisis response requires seamless collaboration between healthcare professionals, emergency responders, and community organizations. Joint training and planning exercises can strengthen these partnerships.
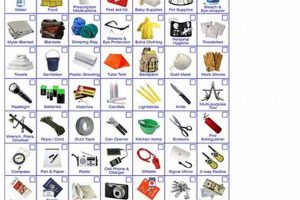
Tip 5: Secure Essential Resources: Maintaining adequate stockpiles of medical supplies, equipment, and pharmaceuticals is crucial. Strategies for procuring additional resources during a disaster should also be established.
Tip 6: Prioritize Mental Health Support: Disasters can have significant psychological impacts on both patients and healthcare providers. Plans must incorporate provisions for mental health services and support systems.
Tip 7: Implement Post-Disaster Evaluation: After a disaster, thorough evaluations are critical for identifying strengths and weaknesses in the response. Lessons learned should inform updates to existing plans and procedures.
By implementing these strategies, healthcare systems can strengthen their capacity to effectively navigate crises, minimize negative impacts, and promote community resilience.
The information provided in this article aims to offer guidance on essential elements of crisis management within healthcare settings. Further research and consultation with relevant experts are encouraged to tailor these principles to specific contexts and needs.
1. Planning
Comprehensive planning forms the cornerstone of effective nursing disaster preparedness. It provides a structured framework for anticipating potential hazards, outlining roles and responsibilities, and establishing procedures for response and recovery. A well-defined plan facilitates coordinated action, minimizes confusion during chaotic events, and maximizes the efficient use of limited resources. Cause-and-effect relationships within disaster scenarios are considered, allowing for preemptive measures to mitigate potential harm. For example, planning for a potential flood might involve pre-positioning essential supplies in locations less susceptible to rising waters, ensuring accessibility even during the disaster’s peak. Planning also allows for the identification of potential vulnerabilities in infrastructure, communication systems, and resource availability, leading to proactive strategies for reinforcement or alternative solutions.
As a crucial component of nursing disaster preparedness, planning enables the development of adaptable strategies for various emergencies, from natural disasters like earthquakes and hurricanes to public health crises such as pandemics. Specific plans may outline procedures for triage, patient evacuation, surge capacity management, and communication protocols. For instance, a plan for a mass casualty incident might detail the roles of different nursing teams, the location and setup of triage areas, and the process for transferring patients to appropriate facilities. Detailed plans, coupled with regular drills and simulations, enhance preparedness, allowing healthcare professionals to respond effectively under pressure and adapt to rapidly evolving circumstances.
Effective disaster planning requires ongoing evaluation and refinement. Lessons learned from previous incidents, changes in community demographics, and advancements in medical technology should inform regular updates to ensure the plan remains relevant and effective. Challenges such as limited resources, communication barriers, and unpredictable disaster dynamics must be addressed proactively during the planning process. Ultimately, robust planning ensures that healthcare systems are well-equipped to provide essential care and support to affected communities, minimizing the negative impact of disasters on public health and safety.
2. Training
Specialized training is paramount for effective nursing disaster preparedness. It equips nurses with the knowledge, skills, and confidence to navigate the complex challenges posed by disaster scenarios. From triage and emergency care to psychological first aid and resource management, comprehensive training ensures a coordinated and effective response, ultimately mitigating the impact of disasters on affected communities.
- Triage and Emergency Care
Training in triage protocols enables nurses to rapidly assess and prioritize patients based on the severity of their injuries or illnesses. This skill is especially crucial in mass casualty incidents, where resources may be limited. Practical exercises and simulations provide hands-on experience in applying triage algorithms, ensuring efficient and equitable allocation of care. For example, training might involve simulated scenarios of a bus crash or a chemical spill, requiring nurses to quickly categorize victims and make critical decisions under pressure.
- Psychological First Aid and Support
Disasters often inflict significant psychological trauma. Training in psychological first aid equips nurses to provide emotional support and coping strategies to both victims and fellow healthcare providers. This training emphasizes active listening, empathy, and the provision of practical information and resources. Recognizing signs of acute stress and post-traumatic stress disorder is also crucial. Training programs might incorporate role-playing exercises to develop skills in providing compassionate care in emotionally charged situations.
- Disaster-Specific Response Protocols
Different types of disasters necessitate specific response protocols. Training tailored to local hazards, such as earthquakes, floods, or industrial accidents, prepares nurses for the unique challenges posed by each scenario. This might include specialized procedures for decontamination, evacuation, or the management of specific injuries. For instance, nurses in coastal regions might receive training in managing injuries related to storm surges and contaminated floodwaters, while those in earthquake-prone areas might focus on treating crush injuries and providing care in unstable environments.
- Resource Management and Logistics
Effective disaster response often requires managing limited resources under challenging conditions. Training in resource allocation, supply chain management, and improvisation is crucial for ensuring efficient utilization of available supplies and equipment. This might involve prioritizing the use of ventilators during a respiratory pandemic or establishing temporary medical facilities in the aftermath of a natural disaster. Training in logistics ensures nurses understand the processes for requesting and distributing resources, coordinating with other agencies, and adapting to changing needs.
These interconnected training components are essential for building a competent and adaptable nursing workforce capable of responding effectively to diverse disaster scenarios. Investing in comprehensive training, coupled with regular drills and exercises, strengthens disaster preparedness within healthcare systems, enhances community resilience, and minimizes the human cost of such events. By equipping nurses with the necessary skills and knowledge, healthcare systems can better protect the health and well-being of their communities in times of crisis.
3. Communication
Effective communication forms the backbone of successful disaster response, particularly within the nursing context. Clear, concise, and timely information flow is crucial for coordinating patient care, resource allocation, and overall situational awareness. Breakdown in communication can lead to delayed responses, misallocation of resources, compromised patient safety, and heightened stress among healthcare providers. For example, during Hurricane Katrina, communication failures hampered evacuation efforts and hindered the delivery of essential medical supplies to affected areas, exacerbating the crisis’s impact on vulnerable populations. Conversely, robust communication systems, as implemented during the 2009 H1N1 pandemic, facilitated the timely dissemination of public health information, enabling effective containment and mitigation strategies. Understanding the cause-and-effect relationship between communication effectiveness and disaster outcomes is paramount for bolstering preparedness.
Several factors contribute to communication challenges during disasters. Overwhelmed communication networks, damaged infrastructure, and the inherent chaos of disaster scenes can disrupt information flow. Varied communication protocols across different agencies and organizations can further complicate coordination. Establishing standardized communication procedures, utilizing redundant communication systems (such as satellite phones and radio), and conducting regular communication drills can mitigate these challenges. Practical applications include establishing clear reporting hierarchies, utilizing standardized terminology for patient status and resource requests, and implementing secure communication channels for sensitive information. Investing in robust communication infrastructure and training healthcare professionals in effective communication strategies strengthens disaster preparedness, enabling a more coordinated and efficient response.
Successfully navigating the complexities of disaster response necessitates prioritizing communication as a core component of nursing disaster preparedness. Effective communication empowers nurses to coordinate patient care, access critical resources, and maintain situational awareness, ultimately improving patient outcomes and mitigating the overall impact of disasters. Addressing communication challenges proactively, through robust planning, training, and investment in reliable technologies, is an essential step towards building more resilient healthcare systems and safeguarding communities against the inevitable disruptions of future disasters. The ability to communicate effectively during a crisis is not merely a logistical detail; it is a fundamental element of effective disaster nursing and a cornerstone of community resilience.
4. Triage
Triage is inextricably linked to effective nursing disaster preparedness, serving as a critical function in resource allocation and patient prioritization during emergencies. The process involves rapidly assessing and categorizing individuals based on the severity of their injuries or illnesses, ensuring that those most in need of immediate medical attention receive it promptly. This systematic approach maximizes the impact of limited resources, particularly in mass casualty incidents where the number of casualties may overwhelm available medical capacity. Cause-and-effect relationships are central to triage: accurate and timely triage decisions directly impact patient outcomes, influencing survival rates and minimizing long-term morbidity. For instance, during the Las Vegas shooting in 2017, effective triage protocols enabled first responders to quickly identify and treat the most critically injured victims, undoubtedly saving lives amidst the chaos. Conversely, inadequate triage procedures during the 2010 Haiti earthquake contributed to delays in care, potentially exacerbating the severity of injuries for some victims.
The importance of triage as a component of nursing disaster preparedness cannot be overstated. Training in established triage systems, such as the Simple Triage and Rapid Treatment (START) method, equips nurses with the skills to make rapid and informed decisions under immense pressure. Regular drills and simulations further reinforce these skills, enhancing proficiency and confidence in applying triage protocols in real-world scenarios. Practical application of triage extends beyond mass casualty incidents; it is equally relevant in other disaster contexts, such as during pandemics or natural disasters. For example, during the COVID-19 pandemic, triage protocols were implemented in hospitals to prioritize patients with severe respiratory distress, ensuring access to limited ventilator resources. The ability to effectively triage patients is not merely a technical skill; it is a cornerstone of ethical and efficient disaster response, directly impacting the allocation of life-saving interventions.
Mastery of triage principles is essential for nurses operating in disaster settings. Challenges to effective triage may include limited information, rapidly evolving situations, and emotional distress among both patients and healthcare providers. Addressing these challenges requires ongoing training, clear communication protocols, and psychological support systems for healthcare workers. Ultimately, integrating triage principles into nursing disaster preparedness frameworks enhances the capacity of healthcare systems to respond effectively to crises, maximizing positive outcomes and minimizing the human cost of disasters. Understanding the direct link between triage effectiveness and disaster outcomes underscores its paramount importance in preparing nurses for the complex demands of emergency response.
5. Resource Allocation
Resource allocation is a critical component of nursing disaster preparedness, directly impacting the effectiveness and efficiency of disaster response. It involves the strategic distribution of essential supplies, equipment, personnel, and facilities to meet the evolving needs of affected populations during emergencies. Cause-and-effect relationships are central to resource allocation decisions: effective allocation maximizes the impact of limited resources, while inefficient allocation can lead to shortages, delays in care, and compromised patient outcomes. The 2011 Tohoku earthquake and tsunami in Japan, for example, highlighted the importance of pre-positioning essential resources and establishing clear allocation protocols. Areas with pre-established supply caches and efficient distribution systems were better equipped to respond to immediate needs, while regions with less developed resource allocation plans faced significant challenges in providing timely aid. Conversely, the inadequate distribution of personal protective equipment (PPE) during the initial stages of the COVID-19 pandemic in some countries underscored the consequences of insufficient resource allocation planning, placing healthcare workers at increased risk and hindering efforts to contain the virus.
The practical significance of understanding resource allocation within the context of nursing disaster preparedness is substantial. Nurses play a key role in assessing needs, requesting supplies, and ensuring the appropriate utilization of available resources. Training in resource management, logistics, and ethical decision-making empowers nurses to make informed choices in challenging circumstances. Practical applications include developing inventory management systems, establishing clear prioritization guidelines for resource distribution, and implementing strategies for resource conservation and reuse. Developing surge capacity plans for personnel and facilities is another critical aspect of resource allocation, ensuring that healthcare systems can accommodate increased patient volumes during disasters. For example, hospitals might establish protocols for converting non-critical care areas into temporary treatment units or for rapidly onboarding additional nursing staff from reserve pools or through mutual aid agreements.
Effective resource allocation is not merely a logistical concern; it is a core element of ethical and effective disaster response. Challenges to optimal resource allocation during disasters may include unpredictable demand surges, disrupted supply chains, and difficult ethical dilemmas regarding resource prioritization. Addressing these challenges requires comprehensive planning, robust communication systems, and ongoing training for healthcare professionals. Integrating resource allocation principles into nursing disaster preparedness frameworks enhances the capacity of healthcare systems to respond effectively and equitably to crises, maximizing positive outcomes for affected communities and minimizing the human cost of disasters. Recognizing the direct link between resource allocation decisions and disaster outcomes underscores the paramount importance of this aspect of preparedness in building resilient healthcare systems.
6. Psychological Support
Psychological support constitutes a crucial element of nursing disaster preparedness, addressing the profound emotional and mental health consequences that often accompany disasters. Beyond physical injuries, disasters can inflict significant psychological trauma on both victims and responders, impacting their ability to cope with the crisis and its aftermath. Integrating psychological support into disaster preparedness frameworks recognizes the interconnectedness of physical and mental well-being, acknowledging that comprehensive care addresses both aspects of human experience. Neglecting psychological support can impede recovery, exacerbate existing mental health conditions, and compromise the overall resilience of individuals and communities. Conversely, providing timely and appropriate psychological support can mitigate the long-term psychological impact of disasters, fostering coping mechanisms and facilitating a return to normalcy.
- Supporting Victims of Disasters
Nurses play a vital role in providing psychological first aid to disaster victims. This involves offering emotional support, practical assistance, and information about available resources. Active listening, empathy, and validation of emotions are crucial components of this support. For example, following Hurricane Katrina, nurses provided psychological first aid to displaced individuals in shelters, offering comfort, reassurance, and practical guidance on accessing essential services. Such interventions can mitigate acute stress reactions, prevent the development of more severe mental health conditions, and foster a sense of hope and resilience among survivors.
- Caring for Healthcare Providers
Disasters can also take a significant toll on the mental health of healthcare providers. Exposure to trauma, long working hours, and the emotional burden of caring for suffering individuals can lead to compassion fatigue, burnout, and secondary traumatic stress. Psychological support for healthcare workers is essential for maintaining their well-being and ensuring their ability to provide effective care. This support may include access to counseling services, peer support groups, stress management training, and opportunities for respite and self-care. For example, during the COVID-19 pandemic, hospitals implemented programs to support the mental health of frontline healthcare workers, recognizing the unprecedented stress and emotional toll of the crisis.
- Community Mental Health Response
Disaster preparedness should encompass community-wide mental health response plans. These plans may involve establishing partnerships with mental health organizations, training community members in psychological first aid, and developing strategies for identifying and supporting individuals at risk for mental health complications. For instance, following the 2011 Fukushima Daiichi nuclear disaster, community mental health programs were implemented to address the psychological impact of the disaster on residents, providing counseling services, support groups, and public education campaigns to promote mental health awareness. Such initiatives are crucial for building community resilience and ensuring access to mental health services for all who need them.
- Long-Term Mental Health Care
The psychological consequences of disasters can extend far beyond the immediate aftermath. Many individuals experience ongoing mental health challenges, such as post-traumatic stress disorder, anxiety, and depression. Disaster preparedness should include provisions for long-term mental health care, ensuring access to appropriate services and support for those affected. This may involve establishing referral networks, developing specialized treatment programs, and integrating mental health services into primary care settings. For example, following the Oklahoma City bombing in 1995, long-term mental health programs were established to provide ongoing support to survivors and families of victims, recognizing the enduring psychological impact of the tragedy.
Integrating psychological support into all facets of nursing disaster preparedness strengthens the overall response and contributes to the long-term recovery of individuals and communities. Recognizing the profound psychological impact of disasters and providing appropriate support are essential components of comprehensive, compassionate, and effective disaster care, ultimately fostering resilience and promoting healing in the face of adversity.
Frequently Asked Questions
This section addresses common inquiries regarding the role of nurses in disaster preparedness and response, aiming to provide clear and informative answers.
Question 1: How does nursing disaster preparedness differ from standard nursing practice?
Disaster preparedness requires specialized knowledge and skills beyond routine patient care. Nurses must be proficient in triage, mass casualty management, psychological first aid, and working within resource-constrained environments. Adaptability and critical thinking are essential in rapidly evolving disaster situations.
Question 2: What specific training is necessary for nurses to be prepared for disasters?
Essential training includes certification in disaster management, advanced cardiac life support, pediatric advanced life support, and psychological first aid. Regular participation in disaster drills and simulations is crucial for reinforcing learned skills and enhancing preparedness.
Question 3: How can nurses contribute to community-level disaster preparedness efforts?
Nurses can participate in community vulnerability assessments, assist in developing local disaster plans, educate community members on disaster preparedness measures, and volunteer with disaster relief organizations. Their expertise in public health and emergency care is invaluable in strengthening community resilience.
Question 4: What ethical dilemmas might nurses face during disaster response?
Disasters often create ethically challenging situations, such as prioritizing limited resources among a large number of casualties, making difficult decisions regarding patient care with limited information, and balancing personal safety with the duty to provide care. Ethical frameworks and established protocols can guide decision-making in these complex circumstances.
Question 5: How can healthcare institutions support nurses in disaster preparedness?
Institutions should provide regular disaster preparedness training, invest in necessary equipment and supplies, establish clear communication protocols, and develop comprehensive disaster plans that include provisions for staff safety and well-being. Supporting nurses’ mental health is crucial, particularly in the aftermath of a disaster.
Question 6: What resources are available to nurses seeking further information on disaster preparedness?
Numerous organizations offer resources and training programs, including the American Red Cross, the Federal Emergency Management Agency (FEMA), and the World Health Organization (WHO). Professional nursing organizations and academic institutions also provide valuable information and educational opportunities related to disaster preparedness.
Preparedness is an ongoing process requiring continuous learning, training, and adaptation. Investing in disaster preparedness is an investment in the resilience of healthcare systems and the well-being of communities.
Further exploration of specific disaster scenarios and response strategies will be provided in the following sections.
Conclusion
Effective management of crises hinges on comprehensive preparation within healthcare systems, particularly emphasizing the crucial role of nurses. This exploration has highlighted key facets of disaster preparedness, encompassing planning, training, communication, triage, resource allocation, and psychological support. Each element is integral to a coordinated and effective response, ultimately minimizing the impact of disasters on affected communities and fostering resilience within the healthcare workforce. Investing in these areas equips nurses to navigate the complexities of disaster scenarios, ensuring timely and appropriate care for those in need.
The increasing frequency and intensity of disasters globally underscore the urgent need for sustained investment in disaster preparedness. Strengthening healthcare systems’ capacity to effectively respond to these events requires ongoing commitment to training, resource allocation, and the development of robust disaster plans. The well-being of communities and the efficacy of disaster response efforts depend on the preparedness of healthcare professionals, particularly nurses who often serve on the front lines of crisis management. Continued focus on these critical areas is essential to building more resilient healthcare systems and safeguarding communities against the inevitable challenges of future disasters.