Emergency preparedness education equips healthcare professionals with the knowledge and skills to effectively respond to various catastrophic events, from natural disasters like hurricanes and earthquakes to public health emergencies such as pandemics. These educational opportunities cover topics ranging from triage and mass casualty care to the management of scarce resources and the psychological impact of disasters on both patients and providers. An example would be a course instructing nurses on how to rapidly assess and categorize patients based on injury severity in a mass casualty incident.
Specialized instruction in disaster response is critical for ensuring a resilient and effective healthcare system. Competent, well-trained nurses are essential for minimizing morbidity and mortality during and after disasters. Historical events, including Hurricane Katrina and the COVID-19 pandemic, have underscored the vital need for healthcare professionals prepared to handle the unique challenges presented by large-scale emergencies. Such training contributes to both individual and community preparedness, enabling nurses to deliver high-quality care even under extreme pressure and resource limitations.
This article will further explore key aspects of disaster preparedness for nursing professionals, including specific curriculum components, available training resources, and the integration of disaster preparedness into standard nursing practice. The information provided will be relevant to nurses at all career stages and in various practice settings.
Disaster Preparedness Tips for Nurses
Preparedness is crucial for effective response in disaster scenarios. The following tips provide guidance for nurses to enhance their disaster readiness.
Tip 1: Familiarize oneself with institutional disaster plans. Understanding the specific procedures, communication channels, and chain of command within one’s healthcare facility is paramount for a coordinated and efficient response.
Tip 2: Maintain up-to-date certifications in basic life support, advanced cardiac life support, and other relevant areas. These skills are fundamental for managing a wide range of medical emergencies that may arise during a disaster.
Tip 3: Develop strong communication skills. Clear and concise communication is essential in stressful situations. Practice communicating effectively with colleagues, patients, and family members in chaotic environments.
Tip 4: Understand the principles of triage and mass casualty care. Disasters often require rapid assessment and prioritization of patients based on the severity of their injuries. Familiarity with these principles is essential for maximizing patient outcomes.
Tip 5: Practice self-care strategies for stress management. Disaster response can be emotionally and physically taxing. Developing coping mechanisms and stress management techniques helps maintain personal well-being and sustain effective performance.
Tip 6: Participate in regular disaster drills and simulations. Hands-on experience through simulated disaster scenarios provides valuable practice and reinforces learned skills, contributing to improved performance in real-world events.
Tip 7: Stay informed about potential hazards and community resources. Awareness of potential risks specific to one’s geographical location and knowledge of available community resources enhances preparedness and facilitates effective response.
By integrating these tips into professional practice, nurses can significantly enhance their ability to effectively and safely respond to disasters, contributing to positive patient outcomes and community resilience.
This information provides a foundation for individual preparedness. Further exploration of specific disaster scenarios and advanced training opportunities are encouraged for continued professional development.
1. Preparedness
Preparedness, a cornerstone of effective disaster management, equips nurses with the necessary knowledge, skills, and resources to effectively respond to emergencies. Within the context of disaster training, preparedness emphasizes proactive planning, training, and resource allocation to mitigate the impact of disasters and ensure a timely and efficient response. This proactive approach minimizes morbidity and mortality, safeguards community well-being, and strengthens healthcare system resilience.
- Individual Preparedness
Individual preparedness focuses on ensuring nurses possess the personal resources and knowledge necessary for self-sufficiency in a disaster scenario. This includes maintaining a personal emergency kit, understanding evacuation routes, and having a family communication plan. For example, a nurse might pack essential medications, first-aid supplies, and copies of important documents in a readily accessible bag. Individual preparedness enables nurses to remain functional and contribute effectively to the response effort even when personal circumstances are disrupted.
- Professional Preparedness
Professional preparedness emphasizes maintaining up-to-date clinical skills, understanding disaster protocols, and participating in regular training exercises. This might involve refreshing advanced life support certifications, familiarizing oneself with hospital disaster plans, and practicing triage procedures. During a pandemic, for instance, a nurse’s professional preparedness would include staying informed on current treatment guidelines and infection control protocols. This preparedness ensures nurses can provide competent and safe patient care in disaster settings.
- Community Preparedness
Community preparedness involves understanding community resources, participating in local disaster drills, and contributing to public health education initiatives. This could include volunteering at community vaccination clinics, assisting with the development of local evacuation plans, or educating community members on disaster preparedness strategies. A nurse might, for example, participate in a community-wide earthquake drill, contributing to the assessment of community vulnerability and response capacity. This engagement builds community resilience and fosters collaboration during disasters.
- Logistical Preparedness
Logistical preparedness focuses on the effective management of resources, supplies, and equipment within healthcare facilities. This includes ensuring adequate stockpiles of essential medications, having backup power systems in place, and establishing efficient supply chain management. For example, a hospital might pre-position emergency generators, stockpile medical supplies, and establish protocols for resource allocation during a hurricane. This proactive approach ensures healthcare facilities can continue to function effectively during and after a disaster.
These facets of preparedness are interconnected and crucial for building a resilient healthcare system capable of withstanding the challenges presented by disasters. By integrating these principles into training programs, nurses develop the necessary skills and mindset to effectively navigate complex emergencies, minimize casualties, and contribute to community recovery.
2. Response
Effective disaster response hinges on the ability of healthcare professionals to rapidly and efficiently deploy resources, provide critical care, and coordinate efforts within a chaotic environment. Disaster training, particularly programs offered through FEMA, equips nurses with the specialized knowledge and skills necessary for successful response operations. This training emphasizes practical application through simulations and drills, fostering adaptability and decisive action under pressure. The connection between effective response and comprehensive training is demonstrably causal: trained personnel consistently exhibit improved performance in real-world disaster scenarios, leading to reduced morbidity and mortality.
Training programs address critical response components, including triage, mass casualty care, communication protocols, and the management of scarce resources. For example, the START triage system, frequently taught in FEMA courses, provides a structured approach to rapidly assess and categorize patients based on injury severity, ensuring that those requiring immediate attention receive it promptly. Furthermore, training emphasizes the importance of clear communication within the Incident Command System (ICS) framework, facilitating coordinated and efficient resource allocation. These skills are essential for navigating the complex logistical and operational challenges inherent in disaster response.
The practical significance of this training is evident in post-disaster analyses. Healthcare systems with well-trained personnel consistently demonstrate improved patient outcomes and more effective resource utilization following disasters. Challenges remain, however, particularly in ensuring consistent access to training and maintaining preparedness over time. Integrating disaster response education into standard nursing curricula and promoting continuing education opportunities are crucial for ensuring a consistently high level of preparedness across the healthcare workforce. This proactive approach is an investment in community resilience and a cornerstone of effective disaster management.
3. Recovery
Recovery, a crucial phase of disaster management, addresses the long-term restoration of physical and emotional well-being, infrastructure, and community functionality following a catastrophic event. Effective recovery requires a multifaceted approach encompassing healthcare system restoration, psychosocial support, and community rebuilding. Training provided through entities such as FEMA plays a vital role in equipping nurses with the necessary skills to navigate the complexities of this phase, contributing to both individual and community resilience. The causal link between comprehensive disaster recovery training and improved community outcomes is well-established, with trained healthcare professionals demonstrating enhanced capacity to address the multifaceted challenges inherent in post-disaster environments.
Training programs often emphasize the importance of psychosocial support during recovery, recognizing the profound emotional impact of disasters on individuals and communities. Nurses trained in psychological first aid, for example, can provide crucial support to those struggling with trauma, loss, and displacement. Furthermore, training equips nurses to address the long-term health consequences of disasters, such as the increased prevalence of chronic illnesses and the need for ongoing rehabilitation services. For example, following Hurricane Katrina, nurses played a vital role in providing ongoing care for individuals with chronic conditions displaced by the storm and in establishing temporary healthcare facilities to address the surge in demand for medical services. The practical application of these skills contributes directly to community well-being and accelerates the recovery process.
While the benefits of disaster recovery training are clear, challenges remain in ensuring consistent access to such programs and in integrating recovery principles into standard nursing practice. Addressing these challenges requires a concerted effort from healthcare institutions, professional organizations, and policymakers. Promoting continuing education opportunities, incorporating disaster recovery into nursing curricula, and developing standardized training protocols are crucial steps toward strengthening community resilience and ensuring a robust healthcare workforce capable of effectively navigating all phases of disaster management. The long-term implications of effective recovery underscore the critical need for ongoing investment in training and preparedness.
4. Mitigation
Mitigation, a crucial element of disaster management, focuses on reducing the potential impact of future disasters. Within the context of FEMA disaster training for nurses, mitigation emphasizes preemptive measures to minimize loss of life, property damage, and disruption to healthcare services. This proactive approach involves identifying potential hazards, implementing strategies to reduce vulnerability, and fostering community resilience. A clear causal relationship exists between effective mitigation efforts and reduced disaster impact, highlighting the critical role of nurses in promoting and implementing these strategies. For instance, training might cover advocating for building codes that enhance structural integrity in earthquake-prone areas or educating communities about flood risks and preventative measures. Such initiatives demonstrate the practical significance of mitigation within disaster preparedness and response.
The practical application of mitigation principles is evident in various disaster scenarios. Following Hurricane Katrina, for example, significant investments were made in strengthening levee systems and improving coastal infrastructure. These mitigation efforts demonstrably reduced the impact of subsequent hurricanes, protecting lives and preserving essential services. Similarly, mitigation plays a crucial role in public health emergencies. Promoting vaccination campaigns and implementing robust infection control measures, as seen during the COVID-19 pandemic, are examples of mitigation strategies that effectively reduce the spread of disease and minimize the burden on healthcare systems. Such real-world examples underscore the critical importance of integrating mitigation into all phases of disaster management.
Integrating mitigation into disaster training for nurses enhances their ability to contribute meaningfully to community resilience. This training equips nurses with the knowledge and skills to identify vulnerabilities, advocate for preventative measures, and educate communities about effective risk reduction strategies. Challenges remain, however, in ensuring consistent application of mitigation principles and in securing adequate funding for these initiatives. Addressing these challenges requires collaborative efforts among healthcare professionals, policymakers, and community stakeholders. Prioritizing mitigation as a core component of disaster management strengthens community preparedness, reduces the long-term costs of disasters, and fosters a more resilient society.
5. Community Engagement
Community engagement represents a critical component of effective disaster preparedness and response. Integrating community engagement into FEMA disaster training for nurses strengthens community resilience and fosters collaborative partnerships essential for navigating the complexities of disaster scenarios. This proactive approach recognizes that successful disaster management requires coordinated efforts across multiple stakeholders, including healthcare professionals, community organizations, and residents. The effectiveness of disaster response is demonstrably linked to the strength of community networks and the level of public preparedness.
- Public Health Education
Public health education initiatives empower communities with the knowledge and skills necessary to prepare for and respond to disasters. Nurses trained in community engagement can effectively disseminate crucial information about disaster preparedness strategies, risk reduction measures, and available resources. For example, nurses might conduct workshops on developing family emergency plans, provide guidance on assembling disaster supply kits, or educate residents about evacuation procedures. These educational efforts contribute significantly to community-wide preparedness and enhance the effectiveness of disaster response.
- Collaborative Partnerships
Building strong collaborative partnerships between healthcare providers, community organizations, and local leaders is essential for coordinating resources and ensuring a unified response during disasters. Nurses trained in community engagement can facilitate these partnerships by participating in community coalitions, establishing communication networks, and fostering relationships with key stakeholders. For example, a nurse might collaborate with a local Red Cross chapter to develop a community-wide emergency shelter plan or work with community leaders to identify vulnerable populations requiring specialized assistance during a disaster. These collaborative efforts enhance communication, streamline resource allocation, and improve overall response efficiency.
- Cultural Competency
Culturally competent disaster response recognizes and addresses the unique needs of diverse communities. Training programs emphasize the importance of understanding cultural sensitivities, language barriers, and specific vulnerabilities within different populations. Nurses trained in culturally competent community engagement can tailor their communication and outreach efforts to effectively reach diverse groups, ensuring that all community members receive appropriate support and resources during a disaster. For example, a nurse might utilize multilingual educational materials or collaborate with community leaders to address culturally specific concerns related to shelter access or healthcare provision. This approach promotes equitable access to essential services and fosters trust between healthcare providers and the communities they serve.
- Post-Disaster Recovery Support
Community engagement extends beyond the immediate response phase of a disaster, playing a crucial role in long-term recovery efforts. Nurses trained in community engagement can contribute to these efforts by participating in community needs assessments, providing psychosocial support, and connecting residents with essential resources. For example, nurses might conduct home visits to assess the needs of vulnerable individuals following a disaster, facilitate support groups for those struggling with emotional trauma, or connect families with housing assistance programs. This sustained engagement contributes to community well-being, promotes resilience, and facilitates a more effective and equitable recovery process.
By integrating these facets of community engagement into FEMA disaster training programs, nurses develop the necessary skills and understanding to effectively collaborate with communities, enhance disaster preparedness, and contribute to more resilient and equitable outcomes in the face of catastrophic events. The demonstrable benefits of community engagement underscore its critical role in comprehensive disaster management.
Frequently Asked Questions
This section addresses common inquiries regarding disaster training for nurses, providing concise and informative responses.
Question 1: What specific skills are taught in disaster training programs for nurses?
Training programs equip nurses with skills in triage, mass casualty care, psychological first aid, emergency communication, and the management of scarce resources. Curriculum content often includes the Incident Command System (ICS), enabling effective collaboration within multi-agency response efforts.
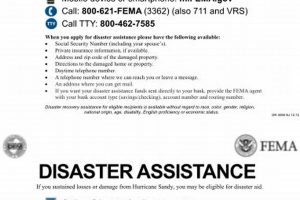
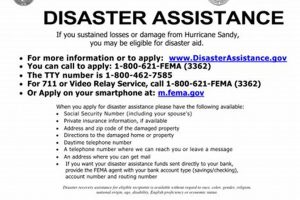
Question 2: How can nurses access FEMA disaster training opportunities?
Information regarding available training courses, schedules, and registration procedures can be found on the FEMA website. Many courses are offered online, providing flexibility for participation. Some healthcare institutions also offer FEMA-certified training programs.
Question 3: Is disaster training mandatory for all nurses?
While not universally mandated, disaster training is strongly encouraged for all nurses, regardless of their practice setting. Preparedness benefits individual nurses, their healthcare institutions, and the communities they serve. Some employers may require specific disaster training for certain roles or departments.
Question 4: How often should nurses refresh their disaster training?
Regularly refreshing disaster training ensures skills and knowledge remain current. Participating in periodic drills and exercises reinforces learned concepts and enhances preparedness. The recommended frequency of refresher training may vary depending on the specific course and individual employer requirements.
Question 5: Does disaster training address the emotional toll of responding to emergencies?
Training programs often incorporate elements of stress management and psychological support. Nurses learn coping mechanisms and self-care strategies to mitigate the emotional impact of disaster response. Recognizing the potential for vicarious trauma and burnout is crucial for maintaining the well-being of healthcare professionals.
Question 6: How does disaster training contribute to community resilience?
Trained nurses play a vital role in enhancing community preparedness and resilience. Through public health education, community engagement, and collaborative partnerships, nurses empower communities to effectively prepare for and respond to disasters, minimizing their impact and fostering recovery.
Preparedness through comprehensive training enhances the capacity of the healthcare system to effectively respond to disasters, minimizing their impact and fostering recovery.
The subsequent section will explore the evolving landscape of disaster management and the ongoing advancements in training methodologies for healthcare professionals.
Conclusion
Specialized instruction in disaster preparedness equips nursing professionals with essential skills and knowledge to effectively navigate the complexities of emergency response. This article explored the core components of such training, encompassing preparedness, response, recovery, mitigation, and community engagement. Each element contributes significantly to individual and community resilience, enabling healthcare systems to withstand and recover from catastrophic events. The examination of real-world disaster scenarios underscored the demonstrable link between comprehensive training and improved outcomes, highlighting the critical role of prepared nurses in minimizing morbidity, mortality, and societal disruption.
Investment in robust disaster training programs represents a commitment to safeguarding communities and fostering a more resilient future. Continued development and refinement of training methodologies, coupled with ongoing research into best practices, remain essential for effectively addressing the evolving challenges of disaster management. The proactive cultivation of a highly trained and adaptable nursing workforce is a critical investment in public health, ensuring that communities have access to skilled and compassionate care in times of crisis.